By Ron Conte, Pharm.D.
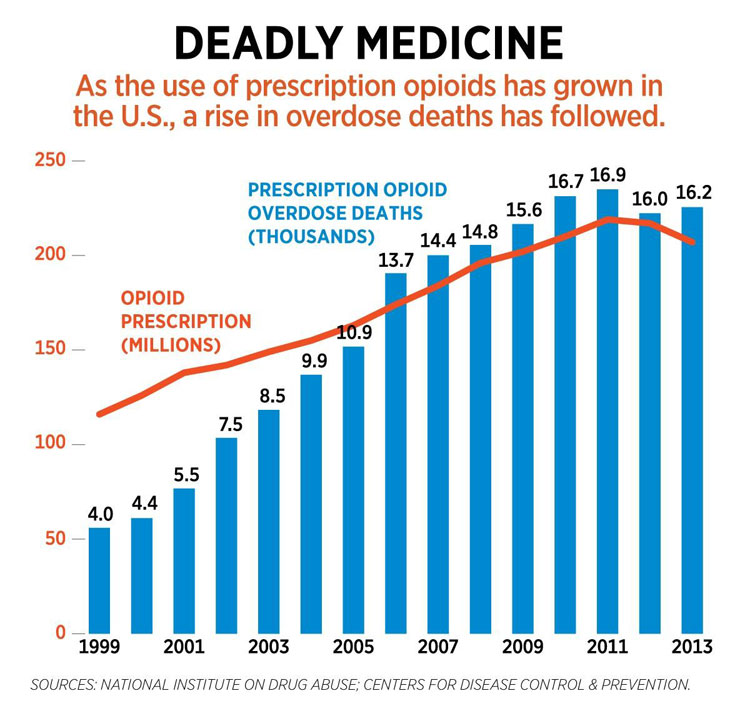
 Opioid prescribing doubled from the late 1990s to 2012. With increased opioid usage come increased misuse and diversion as well as higher rates of deaths due to opioid adverse effects. The word ‘opioid’ describes those drugs that can be derived from opium and possess narcotic effects.
Opioid prescribing doubled from the late 1990s to 2012. With increased opioid usage come increased misuse and diversion as well as higher rates of deaths due to opioid adverse effects. The word ‘opioid’ describes those drugs that can be derived from opium and possess narcotic effects.
From recent accounts, 115 Americans die every day from an overdose of opioids. In 2015, two million Americans were labeled as having an opioid disorder, meaning these individuals took an opioid for non-medical purposes. Almost 30% are classified specifically as having a heroin use disorder. Heroin is an illegal substance in the U.S. How we got to these epidemic numbers is somewhat complex, involving many factors. I will touch upon a few of them, however it is important to start with a basic understanding of opioid effects.
 Opioids are classified as analgesics or pain relievers, commonly referred to as narcotics. Morphine is the prototype by which all other analgesics, even non-narcotics, are compared. From morphine, semi-synthetic opioids, such as buprenorphine, tramadol, and oxycodone, are developed. Narcotics such as levorphanol, methadone, pentazocine, fentanyl, naloxone (generic Narcan), and others, are completely synthetic. Notice that I mentioned naloxone. Although it blocks the effects of opioids, it is still considered a narcotic but does not have pain-relieving properties.
Opioids are classified as analgesics or pain relievers, commonly referred to as narcotics. Morphine is the prototype by which all other analgesics, even non-narcotics, are compared. From morphine, semi-synthetic opioids, such as buprenorphine, tramadol, and oxycodone, are developed. Narcotics such as levorphanol, methadone, pentazocine, fentanyl, naloxone (generic Narcan), and others, are completely synthetic. Notice that I mentioned naloxone. Although it blocks the effects of opioids, it is still considered a narcotic but does not have pain-relieving properties.
Narcotics can be administered by mouth (orally, including under the tongue), subcutaneously (under the skin), transdermally (through the skin by use of a patch), intramuscularly (into a muscle), intravenously (into a vein), epidurally (through a space in the spinal cord), intrathecally (within the cerebrospinal fluid), and intra-articularly (into a knee or shoulder joint). Depending on which narcotic is administered and by which route, the time to onset of pain relief differs.
 Narcotic effects within the human body include a reduction in the conscious level, producing euphoria (a feeling of well-being). This is the reason opioids are termed “drugs of abuse.” In higher doses, opioids can cause respiratory depression (reducing respiratory rate and paralyzing muscles needed for breathing). Death due to a narcotic is due to this respiratory depressant effect, which can be achieved faster if a patient is taking other drugs that cause respiratory depression, e.g., ethyl alcohol.
Narcotic effects within the human body include a reduction in the conscious level, producing euphoria (a feeling of well-being). This is the reason opioids are termed “drugs of abuse.” In higher doses, opioids can cause respiratory depression (reducing respiratory rate and paralyzing muscles needed for breathing). Death due to a narcotic is due to this respiratory depressant effect, which can be achieved faster if a patient is taking other drugs that cause respiratory depression, e.g., ethyl alcohol.
Recent studies show an increase in opioid-induced pneumococcal infections of the lungs that can be quite severe and sometimes fatal. Other narcotic effects include a decrease in blood pressure, constipation, nausea, vomiting, urinary bladder dysfunction, itching, muscle rigidity, and pinpoint pupils of the eyes. If a patient develops a tolerance to a narcotic, the drug may even cause dysphoria (a feeling of dissatisfaction with life).
 When narcotics are taken for longer periods of time and at higher doses, a patient can become addicted and dependent upon these agents. Behavioral science teaches that you cannot separate physical dependence from psychological dependence. Drug dependence is defined as when the body can only function normally in the presence of a drug. If the body is denied that drug, it will react. This is known as withdrawal.
When narcotics are taken for longer periods of time and at higher doses, a patient can become addicted and dependent upon these agents. Behavioral science teaches that you cannot separate physical dependence from psychological dependence. Drug dependence is defined as when the body can only function normally in the presence of a drug. If the body is denied that drug, it will react. This is known as withdrawal.
One factor leading to the opioid crisis is prescribing narcotics for pain that can be treated effectively with non-narcotic agents. Non-narcotic pain relievers include acetaminophen, NSAIDs (Motrin and others), as well as antidepressants (Elavil and others), and anticonvulsants (gabapentin and Lyrica).
There is actually a “stepped-care” approach for treating types of pain. To treat pain quickly and effectively, the origin of pain, location of pain, and whether pain is acute or chronic are important to know. So, for example, nerve pain as in sciatica, may best be treated with an antidepressant. In fact, narcotics are minimally effective in treating nerve pain, fibromyalgia, headaches, low back pain, jaw pain, and irritable bowel syndrome.
A second factor leading to the opioid crisis is in part due to use of long-acting narcotics when short-acting agents will suffice. There is no proof that long acting narcotics are safer or more effective. The risk of overdose is two-times greater with long acting than with shorter acting narcotics.
•••
In my next article (Part II), I will discuss a few other factors contributing to the opioid crisis. I will also discuss a three-pronged approach to deal with the crisis.

