 Pregnancy is a very complex condition. So many factors can disrupt a pregnancy and lead to fetal abnormalities, even death. Drugs could be one of those factors. The study of drugs that may interfere and harm fetal development is known as teratogenicity. This term is used to describe effects of drugs taken by the mother during pregnancy that may cause spontaneous abortion, congenital malformations, mutations, psychomotor abnormalities, or possible carcinogenesis. There are intellectual and behavioral abnormalities that may develop beyond pregnancy, especially with drugs that would eventually affect the central nervous system (brain and spinal cord) of the newborn or infant.
Pregnancy is a very complex condition. So many factors can disrupt a pregnancy and lead to fetal abnormalities, even death. Drugs could be one of those factors. The study of drugs that may interfere and harm fetal development is known as teratogenicity. This term is used to describe effects of drugs taken by the mother during pregnancy that may cause spontaneous abortion, congenital malformations, mutations, psychomotor abnormalities, or possible carcinogenesis. There are intellectual and behavioral abnormalities that may develop beyond pregnancy, especially with drugs that would eventually affect the central nervous system (brain and spinal cord) of the newborn or infant.
The hallmark case of teratogenicity occurred with thalidomide in the 1950’s. This drug was only available in Europe. Thalidomide was an ideal sedative/sleeping medication. However, there were greater than 6,000 cases reported of malformation in newborns of women who took thalidomide during their pregnancy. Thalidomide causes several fetal abnormalities including bone stippling where limbs are stippled with malformations or missing hands and feet. When this drug was being reviewed for general use in the U.S. by the FDA, there were only a few reported cases of thalidomide teratogenicity. One female physician on the review panel who was the deciding vote for thalidomide approval, voted against it.
 Eighty-six per cent of pregnant women will take on average 3 or more drugs during pregnancy. The most common prescription drugs taken include tranquilizers, analgesics, anti-emetics, and antibiotics. Most of them are harmless to the fetus. The literature speaks of a “placental barrier”. What is meant by this is the placenta is selective in what can pass from the mother to the fetus. It really is not a barrier since many substances pass easily by way of the placenta.
Eighty-six per cent of pregnant women will take on average 3 or more drugs during pregnancy. The most common prescription drugs taken include tranquilizers, analgesics, anti-emetics, and antibiotics. Most of them are harmless to the fetus. The literature speaks of a “placental barrier”. What is meant by this is the placenta is selective in what can pass from the mother to the fetus. It really is not a barrier since many substances pass easily by way of the placenta.
There are also changes to the mother during pregnancy that may contribute to how drugs affect the fetus. The mother’s blood circulation increases in volume, but there is a decrease in serum protein. There are also changes in absorption of foods and drugs, quicker elimination of certain drugs from the body, as well as changes in drug metabolism (break down).
 For a drug to pass easily from the mother to the fetus via the placenta, it must be of low molecular weight, fat soluble, and un-ionized (no positive or negative charge). The most crucial phase for drugs passing to the fetus is the first trimester, more specifically the fourth to fourteenth week after conception. During this period there is differentiation of cells with the formation of various organ systems. It is always recommended that women who think they are pregnant, or who become pregnant, consult a healthcare provider to be sure the drugs they are taking during the first trimester are not harmful to her or her fetus.
For a drug to pass easily from the mother to the fetus via the placenta, it must be of low molecular weight, fat soluble, and un-ionized (no positive or negative charge). The most crucial phase for drugs passing to the fetus is the first trimester, more specifically the fourth to fourteenth week after conception. During this period there is differentiation of cells with the formation of various organ systems. It is always recommended that women who think they are pregnant, or who become pregnant, consult a healthcare provider to be sure the drugs they are taking during the first trimester are not harmful to her or her fetus.
The second and third trimester of pregnancy are influenced by Rx dose and the duration of drug effects. For example, a pregnant woman who indulges in drinking alcohol throughout a trimester raises the risk of the baby being born alcohol-dependent. Or, if a non-steroidal anti-inflammatory drug (NSAID) is taken during the second and/or third trimester, there is an increased risk of the baby having heart dysfunction.
I am providing some general guidelines for use of drugs during pregnancy:
- only use medication if absolutely necessary
- avoid use of drugs during the first trimester
- use single agent drug products, not combinations
- use the lowest effective dose
- do not use non-prescription meds that may interfere with Rx drugs
- select medication with proven use during pregnancy
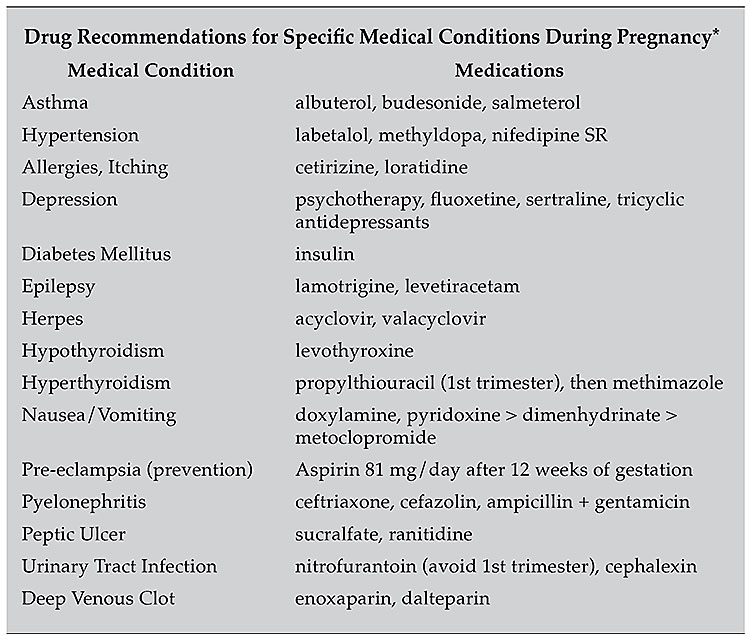
In the table [LOCATION] I have listed drugs that are safe for use during pregnancy. These are recommendations only.
•••
For more info: [email protected]
*Be sure to consult with your healthcare provider before taking any medication or changing your drug therapy regimen

